CAR-T cells for the treatment of blood and solid tumors
T cells with chimeric antigen receptors, more commonly known as CAR-T cells, are used in the immunotherapy of cancer. In CAR-T cell therapy, a patient’s own T cells are taken from their blood and engineered in a laboratory to express an antigen receptor that targets a specific molecule expressed by a patient’s cancer cells. CAR-T cells contain a target-specific extracellular domain fused to the internal domain of CD3-zeta, which may or may not be fused to one or more costimulatory domains. Finally, these cells are transfused back into the patient. These cancer-specific T cells are a powerful tool that track down and kill cancer cells.
The development of CAR-T cells began in the late 1980s-1990s and the technologies that ultimately led to their creation were first developed by immunologists Michel Sadelain and Zelig Eshhar.1,2 At the time the first T cell engineering was taking place, most scientists did not believe that T cells would have much efficacy in the fight against cancer. Little could they have predicted that two decades later, CAR-T cells would be an FDA-approved treatment for adult and childhood cancer.
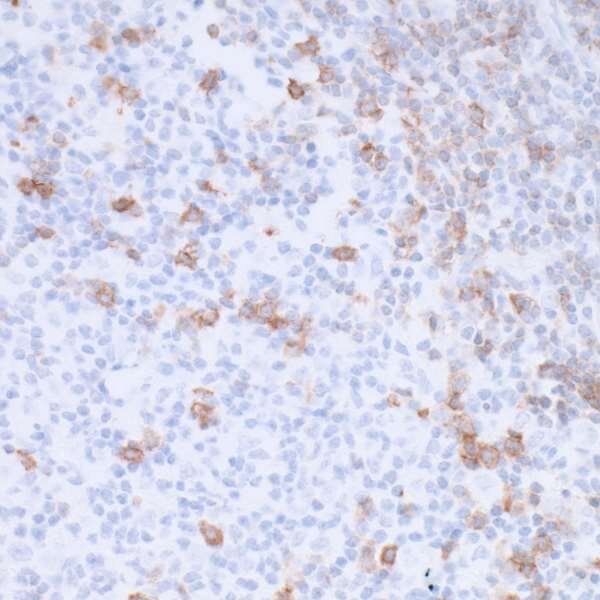
Indeed, the FDA has approved CAR-T cells for the treatment of acute lymphoblastic leukemia, or ALL, in both adults and children, and for the treatment of lymphoma.3 The CAR-T cells used to treat ALL target a molecule called CD19.4 CD19 is found normally on the surface of B cells, where it is involved in B cell development and activation. CD19 is expressed at normal or elevated levels on the malignant B cells of at least 80% of ALL patients, as well as at least 88% of B cell lymphomas and all B cell leukemias, making it a useful therapeutic target in blood cancer. CD19 CAR-T cells are in clinical trials for the treatment of lymphoma and leukemia.
Two types of CD19-targeting CAR-T cells have been developed.5 The first generation CD19 CAR-T cells had just a CD19 recognition domain. However, these cells had a low persistence in vivo and were not very effective as anti-cancer therapy. Second-generation CD19 CAR-T cells added the intracellular domain of a costimulatory molecule: either CD28 or 4-1BB, while third-generation CD19 CAR-T cells include the intracellular domains of both CD28 and 4-1BB, fused to the CD3-zeta intracellular domain. In a clinical trial, a direct comparison of a second- versus third-generation CD19 CAR-T cell for the treatment of lymphoma showed that the third-generation CAR-T cells proliferated and persisted in vivo better than the second-generation CAR-T cells.6 Other studies showed that third-generation CD19 CAR-T cells are also effective against leukemia.7
While CAR-T cell therapy has been extensively evaluated in hematologic malignancies, more recently, CAR-T cells have been developed for some solid tumors as well. For the treatment of neuroblastoma, a childhood cancer that is notoriously difficult to treat, CAR-T cells targeting either GD2 or CD171 have reached clinical trials8. In both cases, some patients had partial or complete responses. Clinical trials for this disease are ongoing. GD2-targeting CAR-T cells have also shown success for the treatment of glioma.9 and are in clinical trials for sarcoma. CAR-T cells targeting HER2, a receptor tyrosine-kinase that is overexpressed in many tumors, have also been explored as a treatment for sarcoma and glioma. In both cancers, some patients showed a clinical response to treatment, which included either stable disease or partial or complete tumor regression10
Multiple other targets of CAR-T cells are also being evaluated for solid tumors, and combination therapies are being explored as well. However, local immune suppression in the microenvironment of solid tumors makes CAR-T therapy more challenging for solid tumors compared to blood tumors. Current clinical trials are exploring the combination of CAR-T cells with checkpoint blockade immunotherapy, which activates the anti-tumor immune response. Early reports from a CAR-T plus anti-PD-1 checkpoint blockade in mesothelioma showed 72% response rate including both partial and complete responses.11
References
- Eshhar Z (2014) From the mouse cage to human therapy: a personal perspective of the emergence of T-bodies/chimeric antigen receptor T cells. Hum Gene Ther 25:773–8 . doi: 10.1089/hum.2014.2532
- Sadelain M, Wang CH, Antoniou M, Grosveld F, Mulligan RC (1995) Generation of a high-titer retroviral vector capable of expressing high levels of the human beta-globin gene. Proc Natl Acad Sci 92:6728–6732 . doi: 10.1073/pnas.92.15.6728
- D’Aloia MM, Zizzari IG, Sacchetti B, Pierelli L, Alimandi M (2018) CAR-T cells: the long and winding road to solid tumors. Cell Death Dis 9:282 . doi: 10.1038/s41419-018-0278-6
- Wang K, Wei G, Liu D (2012) CD19: a biomarker for B cell development, lymphoma diagnosis and therapy. Exp Hematol Oncol 1:36 . doi: 10.1186/2162-3619-1-36
- Park JH, Geyer MB, Brentjens RJ (2016) CD19-targeted CAR T-cell therapeutics for hematologic malignancies: interpreting clinical outcomes to date. Blood 127:3312–20 . doi: 10.1182/blood-2016-02-629063
- Gomes da Silva D, Mukherjee M, Srinivasan M, Dakhova O, Liu H, Grilley B, Gee AP, Neelapu SS, Rooney CM, Heslop HE, Savoldo B, Dotti G, Brenner MK, Mamonkin M, Ramos CA (2016) Direct Comparison of In Vivo Fate of Second and Third-Generation CD19-Specific Chimeric Antigen Receptor (CAR)-T Cells in Patients with B-Cell Lymphoma: Reversal of Toxicity from Tonic Signaling. Blood 128:
- Enblad G, Karlsson H, Gammelgård G, Wenthe J, Lövgren T, Amini RM, Wikstrom KI, Essand M, Savoldo B, Hallböök H, Höglund M, Dotti G, Brenner MK, Hagberg H, Loskog A (2018) A Phase I/IIa Trial Using CD19-Targeted Third-Generation CAR T Cells for Lymphoma and Leukemia. Clin Cancer Res 24:6185–6194 . doi: 10.1158/1078-0432.CCR-18-0426
- Richards RM, Sotillo E, Majzner RG (2018) CAR T Cell Therapy for Neuroblastoma. Front Immunol 9:2380 . doi: 10.3389/fimmu.2018.02380
- Mount CW, Majzner RG, Sundaresh S, Arnold EP, Kadapakkam M, Haile S, Labanieh L, Hulleman E, Woo PJ, Rietberg SP, Vogel H, Monje M, Mackall CL (2018) Potent antitumor efficacy of anti-GD2 CAR T cells in H3-K27M+ diffuse midline gliomas. Nat Med 24:572–579 . doi: 10.1038/s41591-018-0006-x
- DeRenzo C, Krenciute G, Gottschalk S (2018) The Landscape of CAR T Cells Beyond Acute Lymphoblastic Leukemia for Pediatric Solid Tumors. Am Soc Clin Oncol Educ book Am Soc Clin Oncol Annu Meet 38:830–837 . doi: 10.1200/EDBK_200773
- Adusumilli PS, Zauderer MG, Rusch VW, O’Cearbhaill RE, Zhu A, Ngai DA, McGee E, Chintala NK, Messinger JC, Vincent A, Halton EF, Diamonte C, Pineda J, Modi S, Solomon SB, Jones DR, Brentjens RJ, Riviere I, Sadelain M (2019) A phase I clinical trial of malignant pleural disease treated with regionally delivered autologous mesothelin-targeted CAR T cells: Safety and efficacy. In: AACR Annual Meeting. Abstract CT036